Descriptive Study of Acupuncture as an Adjunct Therapy for Patients with Acute Lower Back Pain
Research Article
Tan, Wan Yan Victoria¹, Ho, Chin Ee², Sim, Ann Ling³, Lam, Man Sze⁴, Lee, Wee Yee⁵
¹ ² ³ ⁴ Academy of Chinese Medicine, Singapore, Singapore
³ ⁴ Department of Allied Health, Changi General Hospital, Singapore
⁵ Department of Accident and Emergency, Changi General Hospital, Singapore
Published: 17 May 2025
Abstract
This study evaluates the efficacy of acupuncture as an adjunct treatment for patients with acute lower back pain (LBP) in the Short Stay Unit (SSU) of an emergency department at a public hospital, compared to standard care alone. A total of 68 patients with acute LBP were recruited at Changi General Hospital between May 2019 and March 2023, comprising 46 patients in the Acupuncture Group (AG) and 22 patients in the Control Group (CG). The visual analogue scale (VAS) score decreased by an average of 2.65 points post acupuncture treatment. However, the benefit of a single session of acupuncture as an adjunct therapy was not sustained over a 12-hour observation period. Despite the limitation of a relatively small sample size, the findings provide preliminary evidence supporting the efficacy of acupuncture as an adjunct treatment for acute LBP, therefore expanding treatment options in acute care settings.
Citation: Tan WYV, Ho CE, Sim AL, Lam MS, Lee WY. Descriptive Study of Acupuncture as an Adjunct Therapy for Patients with Acute Lower Back Pain. Journal of Information Systems Engineering & Management. 2025;10(52s):333-340. doi:10.52783/jisem.v10i52s.10717
Introduction
LBP is recognized as a global health concern and the leading cause of disability worldwide [1]. Studies indicate that most individuals experience LBP at some point in their lives, with two-thirds having a recurrence and one-third having periods of disability [2]. Studies have found that LBP poses a tremendous burden to the society in terms of direct healthcare expenses, socio-economic and work absenteeism[3-6]. Acupuncture has been shown to be an effective treatment for both acute and chronic LBP, demonstrating superior pain reduction and improved VAS scores compared to conventional treatments[7,8]. However, limited research exists on its role as an adjuvant therapy, specifically for acute LBP.The objective of this study was to evaluate the use of standard management alone compared to acupuncture as an adjuvant treatment to standard management for the treatment of patients with acute LBP in the acute setting. The primary outcome measure was a decrease in VAS pain score while the secondary outcome was a reduction in turn-inpatient (IP) rates. This study was originally designed as a convenience sampling trial, with the intention to compare 100 patients per arm with moderate exacerbation of acute LBP from the SSU of the Emergency Department in Changi General Hospital. However, due to the Covid-19 pandemic, our study faced recruitment challenges and we managed to recruit 68 patients in total.
Methods
2.1 Study Design and Settings
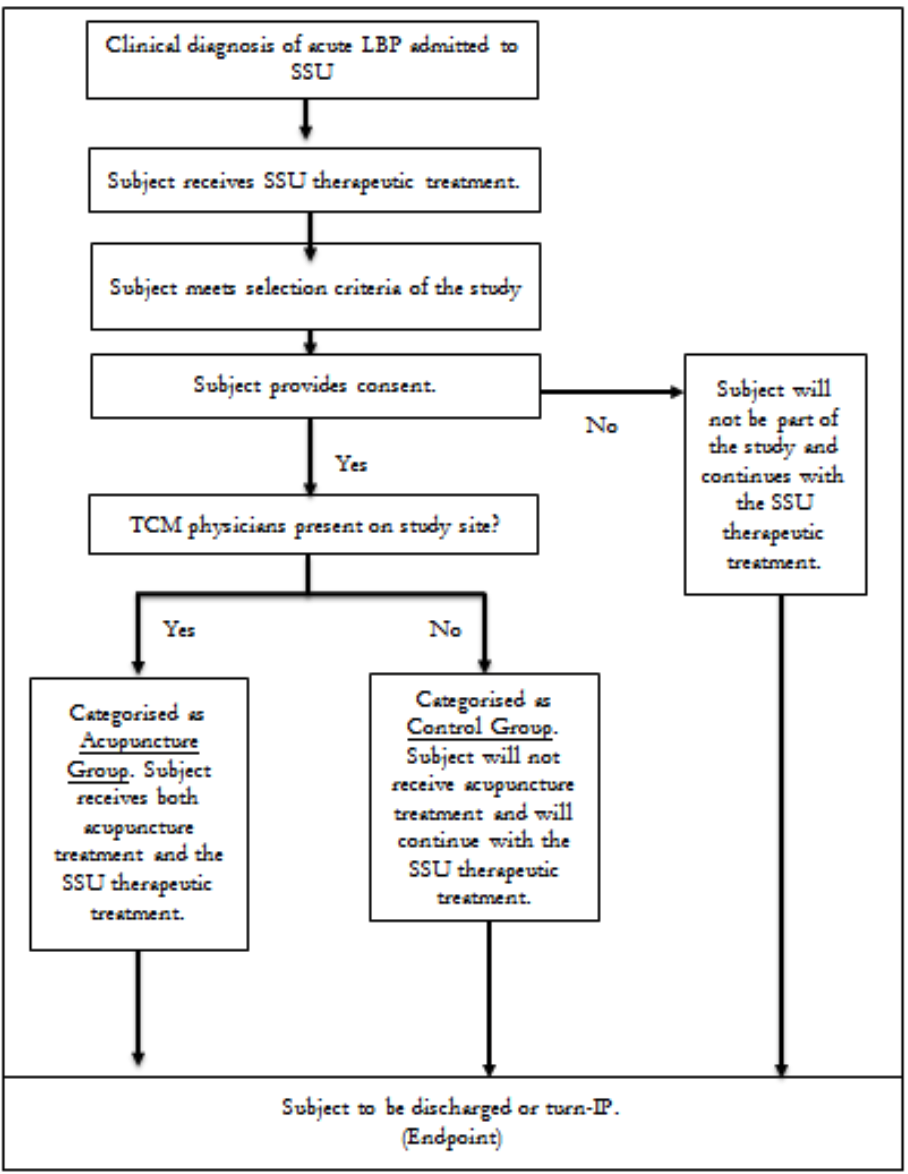
The study is a single-centred, open and treatment-allocated, 2 arm trial, over a period of 2 years and included 68 patients with acute LBP who were admitted to the SSU at CGH between May 2019 and March 2023 (Figure 1). The study team includes SSU doctors who will provide the standard SSU protocol treatment and a team of TCM physicians who will be on-site at specific timing of the week to provide acupuncture treatment to the patients in the Acupuncture Group.
2.2 Participant Selection
Subjects are placed into either the Acupuncture Group (AG) or the Control Group (CG), according to the availability of the TCM physicians on site, as shown in Figure 1. All patients included were informed and provided consent.
Figure 1. Treatment Allocation of Subjects
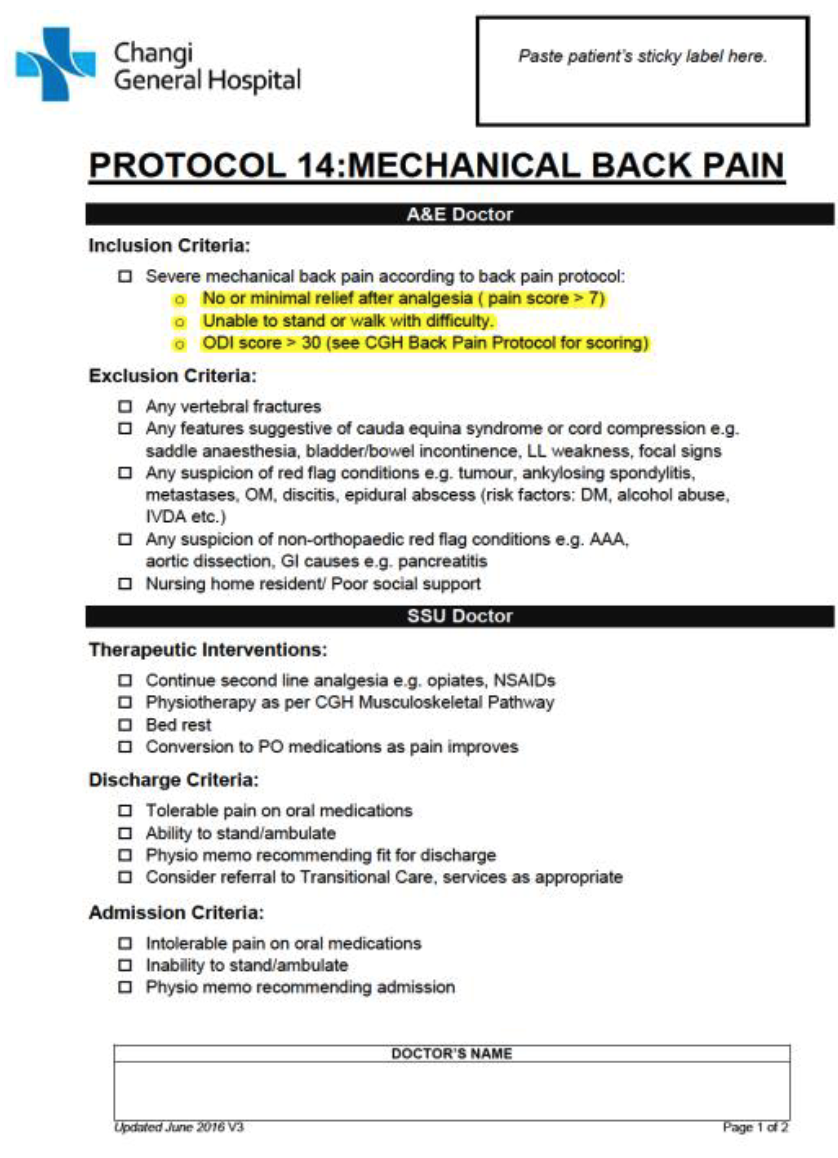
2.3 Inclusion and Exclusion Criteria
2.3.1 Inclusion Criteria
Fulfil the inclusion criteria of SSU Back Pain protocol (Appendix A).
Provision of signed written informed consent ≤ 6 hours from time of SSU admission.
Male or female subjects aged between 21-130 years of age.
Able to communicate with the investigator and to understand and comply with all requirements of study participation.
2.3.2 Exclusion Criteria
Meet the exclusion criteria of SSU Back Pain protocol (Appendix A).
Subjects who declare themselves positive for HIV or viral hepatitis (Hepatitis A, B, C).
Patient’s verbal confirmation of pregnancy.●Refusal to participate or comply with all aspects of the study requirements.
Any condition that, in the opinion of the PI or co-investigator, would complicate or compromise the study or well-being of the subject.
Intervention
3.1 Acupuncture Group
Patients in the AG received one session of acupuncture within 8 hours of their SSU admission. Patients were assessed by an on-site TCM physician using TCM diagnostic methods. The primary acupuncture points selected were: Weizhong (UB40), Shenmai (UB62), Jinmen (UB63), Taixi (KD3), and Yaotongdian (Ex-UE-7). Based on the syndrome differentiation, additional acupuncture points were chosen, including: Yaoyangguan (GV3), Geshu (UB17), Guanyuan (CV4), Qihai (CV6), Xuanzhong (GB39), and Zhaohai (KI6). Additionally, ear seeds were placed on the following acupuncture points on the patients' ears: Kidney, Lumbar Vertebrae, and Sciatic Nerve. The acupuncture needles were left on the patient for 30 minutes, with manual manipulation of the needles.
3.2 Control Group
Patients in this Group received the SSU therapeutic treatment and did not receive any acupuncture treatment.
Statistical Analysis
Descriptive statistics of patient demographics and clinical characteristics were reported as numbers and percentages for categorical data, mean±standard deviation (SD) for normally distributed data, and median and interquartile range (IQR) for non-normally distributed data. The paired t-test was used to determine if there was a change in VAS pain score before and after acupuncture. To explore if patients in the AG had a lower mean VAS pain score at 2, 4, 8, and 12hrs post SSU admission, we performed a multivariable linear regression of the endpoint on group, adjusting for the outcome at admission. The adjusted, unstandardized beta coefficients of the group with corresponding 95% confidence intervals (CIs) were reported. Logistic regression was used to estimate the odds of inpatient admission in the AG relative to that in the CG. Statistical tests were two-sided with a 0.05 significance level. All statistical analyses were conducted using Stata 18 (College Station, TX: StataCorp LLC).
Results
5.1 Sample Characteristics
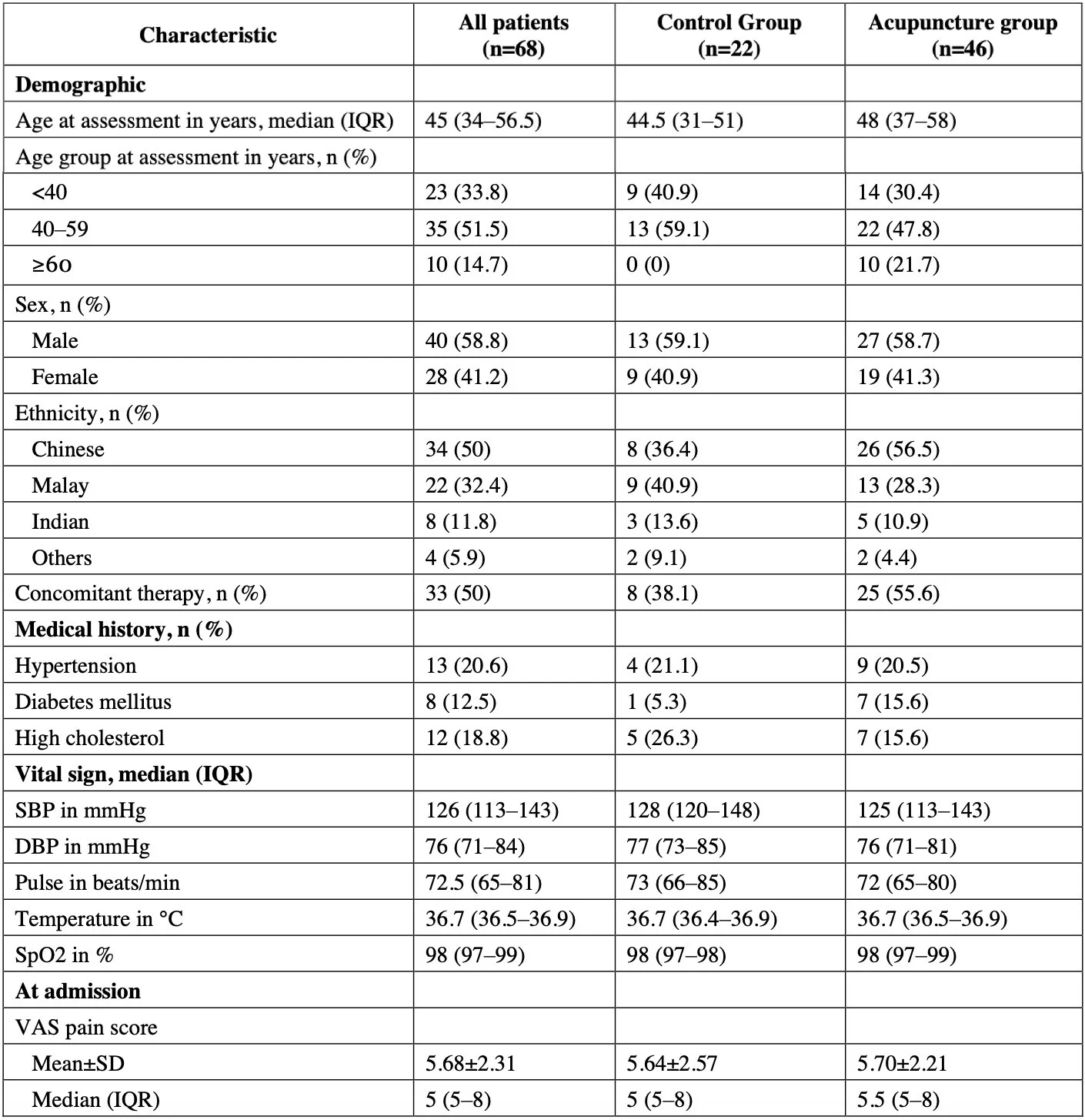
A total of 68 patients who had a clinical diagnosis of lower back pain and who were admitted to SSU were included. 22 patients were allocated to the CG to receive standard treatment only, while 46 patients were allocated to the AG to receive both standard treatment and acupuncture as an adjunct treatment. The overall median age at assessment was 45 years (IQR 34–56.5) and 41.2% (28/68) of patients were female. Patients in the AG appeared more likely to be older, Chinese, have concomitant therapy and a history of diabetes mellitus, but less likely to have a history of high cholesterol compared to patients in the CG (table 1).
Table 1. Baseline patient demographic and clinical characteristics, by treatment group
DBP=Diastolic blood pressure. IQR=Interquartile range. SBP=Systolic blood pressure. SD=Standard deviation. SpO2=Oxygen saturation. VAS=Visual analogue scale.
5.2 VAS Pain Score
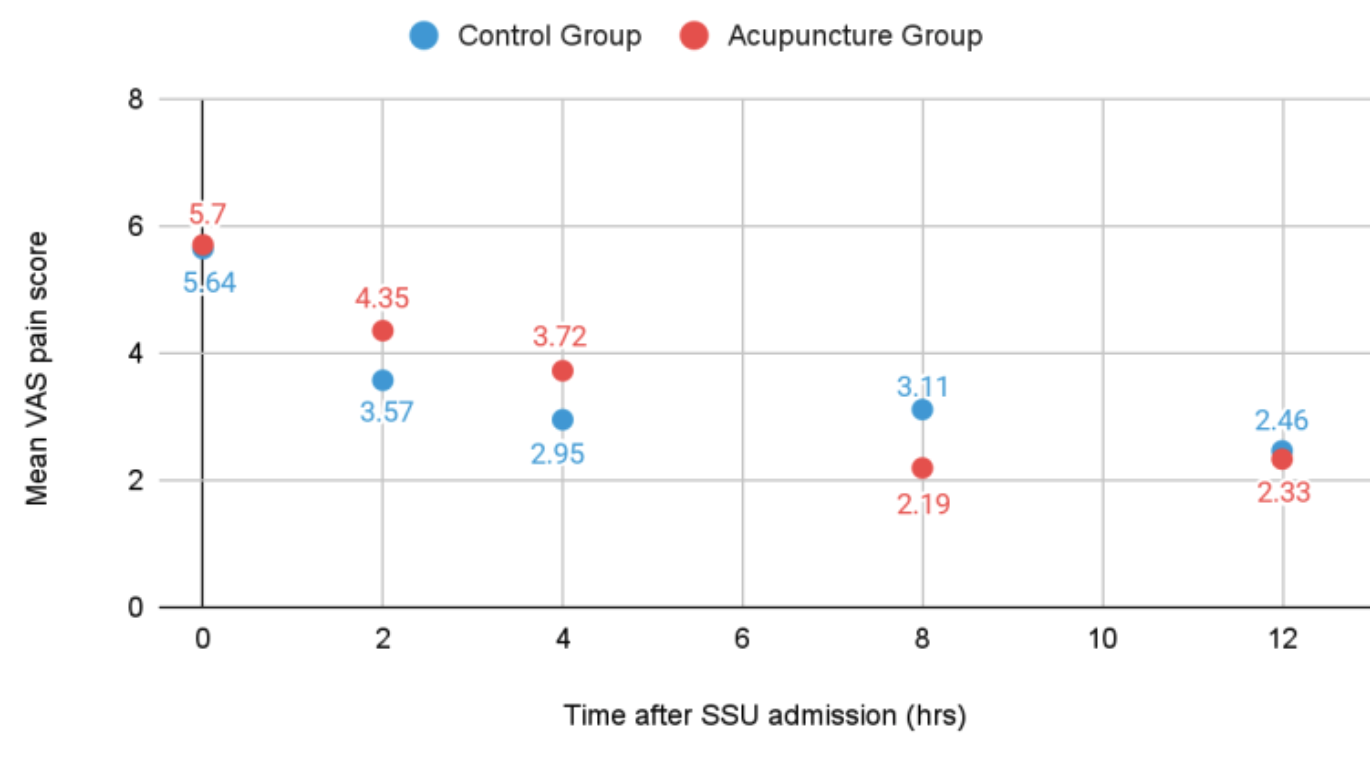
The mean VAS pain score at SSU admission among patients in the CG and AG was 5.64±2.57and 5.70±2.21 respectively. The change in mean VAS pain score across time between AG and CG is displayed in graph 1.
Graph 1: Estimated effect of group on endpoints across time
The mean score immediately before and after acupuncture in AG was 6.85±2.04 and 4.20±2.08 respectively. The mean difference was -2.65 (95% CI -3.14 to -2.16, paired t-test P<0.001.
5.3 Status of Disposition
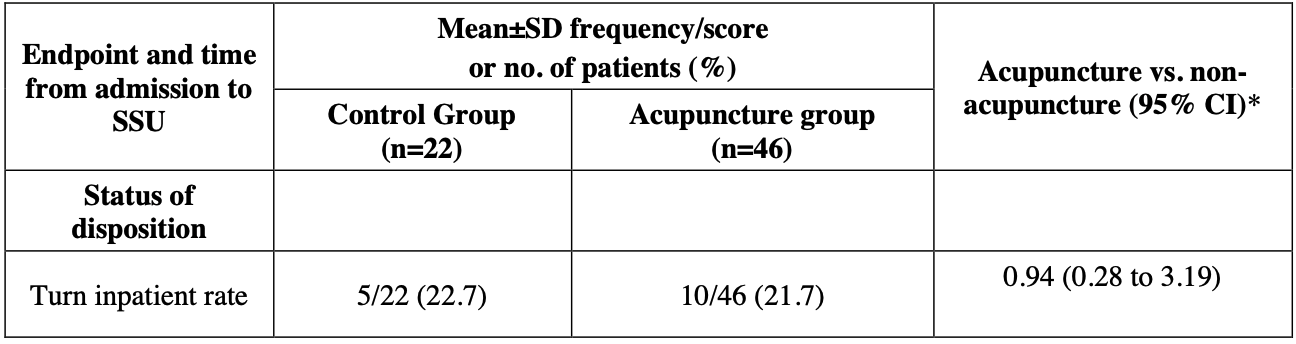
5 of 22 (22.7%) patients in the CG turn-IP, compared to 10 of 46 (21.7%) patients in the AG (Table 2).
Table 2. Estimated effect of group on endpoints across time.
*Estimated difference in mean endpoint post SSU admission between AG and CG, after adjusting for outcome at SSU admission. For status of disposition, the odds ratio was estimated using logistic regression.
CI=Confidence interval. SD=Standard deviation. SSU=Short Stay Unit. VAS=Visual analogue scale
5.4 TCM Classification of Patients with Lower Back Pain
Patients were classified under blood stasis syndrome (43%), followed by cold dampness (22%), deficiency in kidney Yang (20%), deficiency in kidney Yin (11%) and others (4.3%).
Discussion
Overcrowding at the Accident and Emergency (A&E) of hospitals and hospital bed crunch has always been an issue in Singapore and worldwide. In this study, we explored the efficacy of acupuncture as an adjunct therapy to the standard management protocol for symptomatic relief and IP turnover rate. This study suggests that a single acupuncture session can provide significant immediate relief for acute lower back pain. Notably, the mean VAS score immediately before and after acupuncture was 6.85 and 4.20 respectively, with a statistically significant decrease of 2.65 points in pain score. However, when comparing the VAS pain score trend over a period of 12 hours, the difference in effectiveness between the two groups is minimal. There is also no difference in the SSU turn IP rate between the two groups and hence no mid-term advantage for a single session of acupuncture to be administered as an adjunct treatment for acute LBP.
For TCM Syndrome, we observed that most of the patients were classified under blood stasis syndrome (43%), followed by cold dampness (22%), deficiency in kidney Yang (20%) and deficiency in kidney Yin (11%). This is in accordance with TCM’s view of acute lower back pain which is a manifestation of imbalances in the body’s Qi and blood circulation. Poor posture, injury or trauma can disrupt the flow of Qi and blood in the lower back, leading to blood stasis, which when left untreated, will result in a sharp ,localised pain in the lower back. The second most common classification is deficiency in kidney Yang. Due to Singapore’s hot and humid weather, air conditioning is commonly used. Prolonged exposure to this environment can result in the invasion of cold and dampness pathogens, thereby leading to back pain. In TCM, the kidney Qi starts becoming deficient from middle age onwards. For middle-aged adults, a prolonged exposure to an air conditioned environment further weakens the Yang, thus resulting in deficiency in kidney Yang and lower back pain.
This was a single-centred study which may not be representative of the general population of Singapore. The difference in sample characteristics, in terms of age distribution and comorbidities, may have impacted the accuracy of the results. The disruption of the study due to the COVID-19 pandemic was unfortunate as this has reduced the power of the study substantially. Nonetheless, the study has generated important preliminary data for the design of future robust trials to examine the efficacy of acupuncture for the management of acute LBP.
Conclusion
Overall, the result obtained from this study is different from other studies. Although there is an improvement in VAS score immediately post acupuncture, over a 12 hour period, there is no advantage of using a single session acupuncture as an adjunct therapy for management of acute LBP. In our study in Singapore, the majority of the patients were found to be classified under blood stasis syndrome (43%).
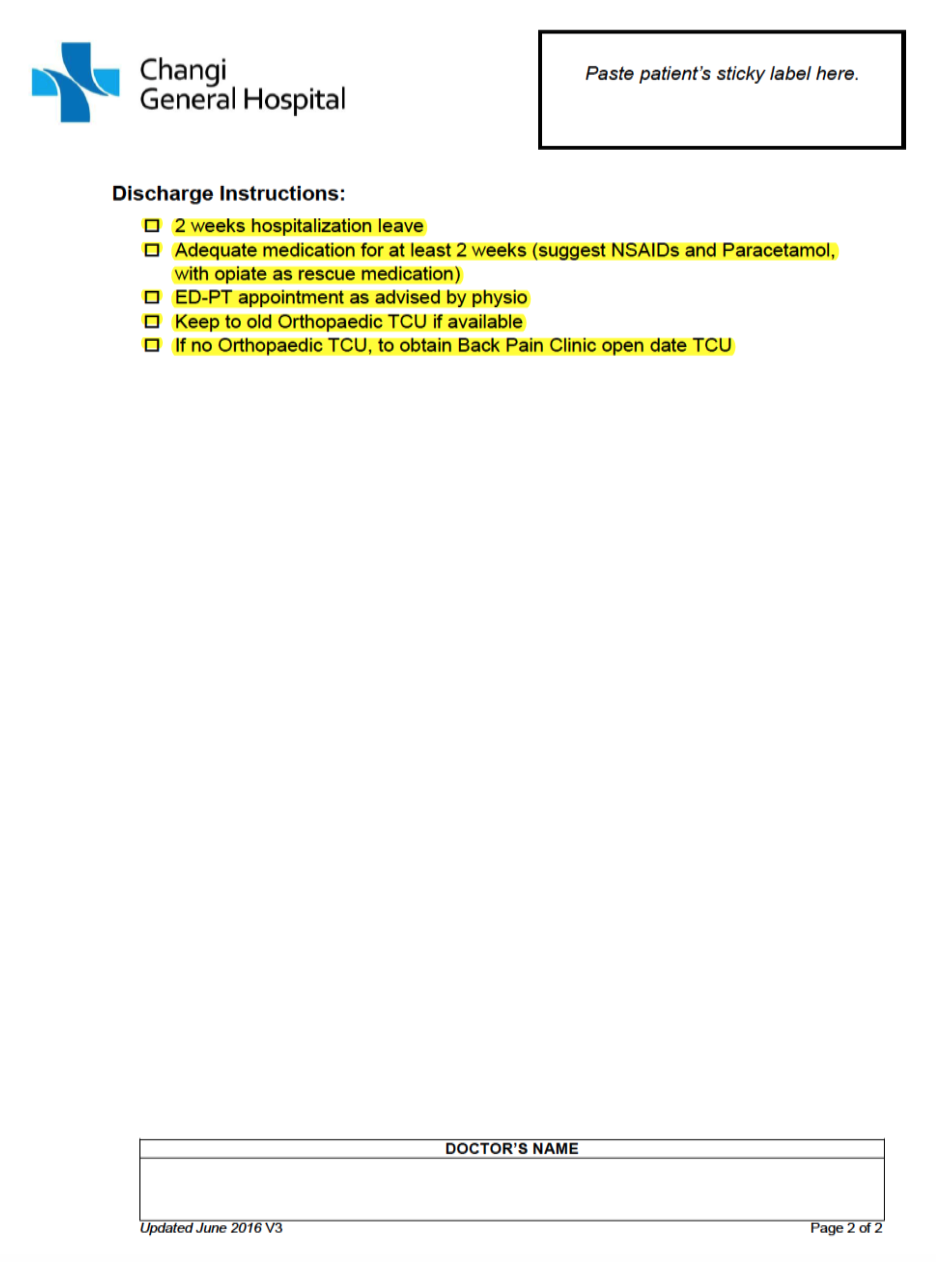
Appendix
Appendix A. SSU Back Pain Protocol
Acknowledgements
The authors would like to thank Clinical Trials and Research Unit, CGH, Academy of Chinese Medicine Singapore and Dr Tiah Ling (Emergency Department, CGH) and Mr Koh Xuan Han (Analyst, CGH Health Services Research), for their assistance and support in this research.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
[Article in a journal] Murray, C.J., et al., Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet, 2012. 380(9859): p. 2197-223.
[Article in a journal] Haldeman, S., et al., Advancements in the management of spine disorders. Best Pract Res Clin Rheumatol, 2012. 26(2): p. 263-80.
[Article in a journal] Hoy, D., et al., The Epidemiology of low back pain. Best Pract Res Clin Rheumatol, 2010. 24(6): p. 769-81. factors. Eur Spine J, 2012. 21(7): p. 1234-40.
[Article in a journal] Juniper, M., T.K. Le, and D. Mladsi, The epidemiology, economic burden, and pharmacological treatment of chronic low back pain in France, Germany, Italy, Spain and the UK: a literature-based review. Expert Opin Pharmacother, 2009. 10(16): p. 2581-92.
[Article in a journal] Ekman, M., O. Johnell, and L. Lidgren, The economic cost of low back pain in Sweden in 2001. Acta Orthop, 2005. 76(2): p. 275-84.
[Article in a journal] Walker, B.F., R. Muller, and W.D. Grant, Low back pain in Australian adults: the economic burden. Asia Pac J Public Health, 2003. 15(2): p. 79-87.
[Article in a journal] Liu, Y.T., et al., Efficacy and Safety of Acupuncture for Acute Low Back Pain in Emergency Department: A Pilot Cohort Study. Evid Based Complement Alternat Med, 2015. 2015: p. 179731.
[Article in a journal] Haake, M., et al., German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med, 2007. 167(17): p. 1892-8.